Redefining substances: The Difference Psychedelics, Cannabis & “Hard Drugs”
Chapter 4: What are Psychedelics?
Psychedelics 101 Series
Understanding the Fundamentals of Psychedelics
Estimated reading time: 9 mins
June 15, 2023
Table of Contents
In the previous article: “Psychedelics in Western Medicine: Pharmacology”, we explored the basic pharmacology of these substances. Now you enter the second half of Chapter 2, equipped to understand the difference between psychedelics, cannabis & “hard drugs”.
Is cannabis a psychedelic substance?
Cannabis and psychedelics may seem similar at first glance, both altering perception, mood, and cognitive processes, and being used for therapeutic, recreational, and spiritual purposes. But when taking a closer look, the differences between cannabis and psychedelics become clear.
Psychedelics and cannabis act on different receptors and neural pathways in the brain. While classical psychedelics interact with the serotonergic system in the brain, cannabis interacts with the endocannabinoid system, specifically the CB1 and CB2 receptors.
The experiential effects differ, too. While the effects of cannabis are usually more calming and sedating, the classic psychedelic substances can lead to more pronounced and revealing states, such as the “dissolution of the boundaries of the self”.
The therapeutic application of these substances also differs. Cannabis is most commonly used to treat chronic pain and spasticity whereas serotonergic psychedelics have been studied for the treatment of treatment-resistant depression, PTSD, and addiction/substance abuse. Similar to psychedelics, cannabis is increasingly used in therapeutic settings to treat PTSD [1]. It is likely that the scope of clinical applications for both substances will be widened in the future.
Hard drugs and Psychedelics do not belong in the same box
In the previous article in this series, we explored the tendency of policy-makers – which has been vehemently opposed by many scientists – of tossing psychedelics into the same bucket together with actually harmful substances, or “hard drugs”, like heroin, cocaine, crack, or crystal meth. Actually, “hard drugs” and psychedelics are very different in important ways. Here we cover important risk differences related to addictive potential, physiological toxicity and psychological safety.
Addictive potential
Hard drugs are dangerous because they are highly addictive, causing severe physical and psychological dependence. The addictive potential of hard drugs comes from their strong manipulation of the dopamine system in the brain [2]. From an evolutionary perspective, this system has evolved to motivate us to take action that serves our survival, such as eating and having sex, by providing the reward of pleasure through the release of dopamine [3]. Hard drugs artificially hijack this system by drastically boosting the production of dopamine and other neurotransmitters beyond natural levels, tricking the brain into believing it is taking a useful action by creating a disproportionately high dopaminergic reward without the need for effort. This leads to compulsive drug-seeking behavior and intense withdrawal symptoms when trying to quit using.
Unlike hard drugs, classic serotonergic psychedelics do not interact with the brain’s dopamine system [4]. A body of research has confirmed that after a psychedelic experience, there is no craving to repeat it or want more as it does not cause dependence or addiction. In fact, the vastness and intensity of the psychedelic experience often has the opposite effect, causing people to stay away from psychedelics in order to integrate and make sense of the experience.
Actually, opposite to being addictive substances, psychedelics used in the right context, have shown their potential in treating substance abuse disorders (addiction) like alcoholism [5].
Toxicity
For almost half a century, mainstream media has neatly played along the political agenda of the War on Drugs, and has painted psychedelics as dangerous and harmful substances. Various unsubstantiated claims about the toxicity of psychedelics were made, for instance, that LSD would damage people’s chromosomes. In fact, classic serotonergic psychedelics are non-toxic for the liver and the central nervous system, even in very high doses [6]. It may be surprising to many but every bottle of beer sipped on a warm summer day or a cigarette casually smoked during the coffee break is considerably more harmful in terms of toxicity than a journey on a classic serotonergic psychedelic. In a state-of-the-art pharmacological review, world-renowned professor Nichols summarized that “…from a physiologic standpoint they [psychedelics] are in fact one of the safest known classes of CNS drugs” [7].
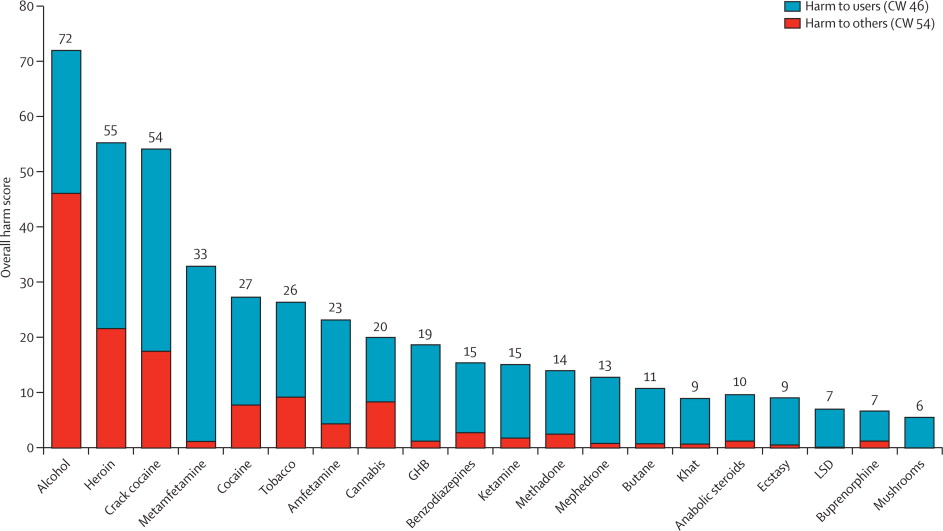
Moreover, scientific research found that psychedelics are much less harmful to the user and society compared to commonly accepted drugs like alcohol and almost all other controlled substances [8]. A study published in the world’s most prestigious medical journal The Lancet by Nutt and colleagues claimed that heroin, crack cocaine, and metamfetamine were the most harmful drugs to individuals, whereas alcohol, heroin, and crack cocaine were the most harmful to others. LSD and mushrooms, on the contrary, were found to be the least harmful of all substances (see graph below).
As opposed to serotonergic psychedelics, hard drugs can cause significant toxicity to the body. The exact effects vary depending on the specific drug and the individual’s use pattern. However, some common physiological effects of hard drug use include damage to the heart, lungs, liver, and kidneys. Cocaine and methamphetamine use, for example, can cause heart attacks, high blood pressure, and stroke [10]. Heroin and opioid use can lead to respiratory depression, which can cause oxygen deprivation and death. Hard drugs can also alter the brain’s chemistry and structure, leading to changes in behavior, mood, and cognitive function, and pathological decreases in the size of certain brain regions.
Psychological safety
Hard drugs, such as cocaine, methamphetamine, and others, can contribute to the development of mental health disorders, such as depression and anxiety. Hard drugs can impair cognitive function and memory, leading to difficulty in thinking clearly and performing everyday tasks. The risk of developing paranoia and delusions, as well as experiencing mood swings, also are also frequently associated with hard drug use.
While certain psychedelics are considered to be safe from a physiological standpoint, it’s important to remember that they can still impair judgment and decision-making abilities during the experience [11]. Therefore, the importance of preparation, supervision, support, and integration work, either in a clinical or traditional ceremonial context, cannot be overstated. What’s more, following an impactful psychedelic experience, it is advised to delay taking important and drastic life decisions for a few weeks or months.
Another risk to keep in mind is the potential of psychedelics to trigger psychotic episodes in rare instances. This risk can be greatly reduced with psychiatric screening beforehand, mindset preparation, and the right physical setting. When these factors are considered, a psychedelic journey can be considered a reasonably safe experience. In a recent review of the scientific literature, Schlag et al. concluded that “many–albeit not all–of the persistent negative perceptions of psychological risks are unsupported by the currently available scientific evidence” [12].
We discussed the differences and similarities between psychedelics, cannabis, and “hard drugs” in terms of their pharmacology, effects, and therapeutic potential. While cannabis and psychedelics share some similarities in terms of their effects on perception, mood, and cognition, they act on different receptors and neural pathways in the brain. Additionally, they have different therapeutic applications, with cannabis commonly used to treat chronic pain and spasticity, and psychedelics studied for the treatment of treatment-resistant depression, PTSD, and addiction/substance abuse. “Hard drugs,” on the other hand, are dangerous because of their high addictive potential and physiological toxicity, which can cause damage to the heart, lungs, liver, and kidneys. In contrast, psychedelics have been shown to be non-addictive and non-toxic, making them one of the safest known classes of CNS drugs. Overall, this article emphasizes the importance of separating psychedelics from “hard drugs” and reconsidering the way they are categorized and regulated.
Please bear in mind that we do not provide medical advise and you should always seek assistance from a medical professional before making any decision about consuming psychedelics.
Ready for a paradigm shift?
The next article “Psychedelics and Reality: It’s Time for a Paradigm Shift” is of a different nature, as it opens the possibilities of interpreting the psychedelic experience through an exploration of metaphysics and the concept of the paradigm shift.
Images
Uncited images were created by Nino Galvez using AI image generators
References:
[1] Rehman, Y., Saini, A., Huang, S., Sood, E., Gill, R., & Yanikomeroglu, S. (2021). Cannabis in the management of PTSD: A systematic review. AIMS Neuroscience, 8(3), 414–434. https://doi.org/10.3934/neuroscience.2021022
[2] Wise, R. A., & Robble, M. A. (2020). Dopamine and addiction. Annual Review of Psychology, 71(1), 79–106. https://doi.org/10.1146/annurev-psych-010418-103337
[3] Adamson, S., Sellman, D., & Durrant, R. (n.d.). Drug use and addiction: Evolutionary perspective. Retrieved April 11, 2023, from https://journals.sagepub.com/stoken/default+domain/KSSZgznJHBs2jjuysanV/full
[4] Nichols, D. E. (2016, April). Psychedelics. Pharmacological reviews. Retrieved April 11, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4813425/
[5] Stone AL, Storr CL, Anthony JC (2006). Evidence for a hallucinogen dependence syndrome developing soon after onset of hallucinogen use during adolescence. International Journal of Methods in Psychiatric Research, 15(3), 116–130.
[6] Anne K. Schlag, Jacob Aday, Iram Salam, Jo C. Neill and David J.Nutt (2022) Adverse effects of psychedelics: From anecdotes and misinformation to systematic science. Journal of Psychopharmacology, 36(3), 258–272. https://doi.org/10.1177/02698811211069100
[7] Nichols, D. E. (2016, April). Psychedelics. Pharmacological reviews. Retrieved April 11, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4813425/
[8] Nutt, D., King, L. A., Saulsbury, W., & Blakemore, C. (2007). Development of a rational scale to assess the harm of drugs of potential misuse. The Lancet, 369(9566), 1047–1053. https://doi.org/10.1016/s0140-6736(07)60464-4
[9] Nutt, D. J., King, L. A., & Phillips, L. D. (2010). Drug harms in the UK: a multicriteria decision analysis. The Lancet, 376(9752), 1558–1565. doi:10.1016/s0140-6736(10)61462-6
[10] Lee, C. Y. S., Mohammadi, H., & Dixon, R. A. (1991). Medical and dental implications of cocaine abuse. Journal of Oral and Maxillofacial Surgery, 49(3), 290–293. https://doi.org/10.1016/0278-2391(91)90223-9
[11] Reynolds, P. C., & Jindrich, E. J. (1985). A mescaline associated fatality. Journal of Analytical Toxicology, 9(4), 183–184. https://doi.org/10.1093/jat/9.4.183
[12] Schlag, A. K., Aday, J., Salam, I., Neill, J. C., & Nutt, D. J. (2022). Adverse effects of psychedelics: From anecdotes and misinformation to systematic science. Journal of Psychopharmacology, 36(3), 258–272. https://doi.org/10.1177/02698811211069100
Subscribe to the insights newsletter
At most, once every 2 weeks.