Dr. Martha Havenith
This article was written by Dr. Martha Havenith and Dr. Abdel Nemri
Using your breath to change your mind: A neuroscience view on breathwork
‘I saw the line of my ancestors stretching out before me, and the qualities they had passed on through the family line – talents, loves, burdens… I also felt where the line was broken by trauma. I realized that in healing myself, I was also healing my ancestors, and that I need that connection to act in this world. I felt that I was sending compassion throughout the ancestral line and also to myself as its newest link, and energy started flowing towards me from my elders.’
If you happen to be familiar with psychedelic experiences, this description might remind you of an Ayahuasca or Psilocybin journey. It also wouldn’t seem out of place in a religious trance – or even just a very vivid dream. But as you can probably guess from the title of this post, it’s none of the above. What you just read is the description of a circular breathwork experience. Circular breathwork comes in a whole host of flavours like conscious-connected, holotropic, transformational, shamanic and rebirthing breathwork. What unites all these practices is the same simple breathing technique at their core: You breathe deeply into your belly, at a slightly faster pace than usually; and you don’t take breaks, meaning that you connect inhale and exhale into a circle. And then you just keep doing that – for anywhere from 15 minutes to several hours. That’s it! And yet, this simple breathing pattern can open up some pretty unusual spaces in your mind. It may resurface childhood memories, conjure up visual experiences, trigger intense emotions, or reveal and shake up deep-seated patterns of thought and feeling.
Now, not every breathwork experience will immediately be a firework of deeply memorable impressions. In fact, the first effects you may notice as you start your session may not feel all that impressive: You may feel a bit light-headed, find it hard to focus, and your skin may tingle. You may also experience some mild to annoying muscle cramps e.g. in your hands or jaw (referred to as tetany). So far, so unspectacular. But as you move deeper into the session, more interesting things will usually start to happen. You may find yourself crying, screaming or laughing spontaneously, feel your body move or shake in ways that you didn’t plan, experience sudden ‘Aha!’ moments and unexpected1 cognitive insights, flashbacks to past events, or imaginary encounters in which you can clearly see, hear or touch things that are not physically present. On the less dramatic end of things, you may wrestle with thoughts like ‚Am I doing this right?‘…. or simply fall asleep!
Whatever the unique mix of experiences in a session, it’s generally not the type of thing you’d expect to happen while you are browsing shelves at the supermarket. This departure from everyday consciousness makes breathwork part of the family of non-ordinary states of consciousness (NOSCs). NOSCs are simply defined as any mental state that clearly deviates from typical waking consciousness. This includes e.g. dreaming, meditation, hypnosis, trance, as well as psychedelic and near-death experiences [1]-[3]. Out of this family, breathwork‘s closest relatives are probably psychedelic and hypnotic states, as well as other forms of mystical and trance experiences [2]. In fact, when they are measured by questionnaires typically used to quantify psychedelic states, breathwork experiences are often hard to distinguish e.g. from a psilocybin trip [4]-[5]. So how does altered breath create altered consciousness? To answer this question, we will have to go on a bit of a treasure hunt, following the breadcrumbs from the known physiology of intense breathing to its largely unknown effects on the brain. Let’s explore!
Breathwork and the body
The neuronal dynamics of breathwork may still be a bit of a riddle, but its physiological effects are much clearer. Not because physiologists are wildly studying breathwork, but because breathwork is just about similar enough to medically researched forms of hyperventilation like e.g. the ones you see in panic attacks. Now, that doesn’t mean they’re the same! For instance, during a panic attack your breathing will often be fast but shallow. In contrast, during breathwork, you breathe intensely but deeply, engaging both activating and relaxing signals in your brain. Similarly, during a panic attack, the stress centres in your brain, like amygdala and hypothalamus, will be highly active. In contrast, you would ideally enter a breathwork session feeling relaxed and curious, so that your brain’s stress centres should be pretty quiet. Nevertheless, the overlap between circular breathwork and ‘bad’ hyperventilation is big enough that it can help us understand the basic workings of breathwork in the body. Here goes:
Breath and blood
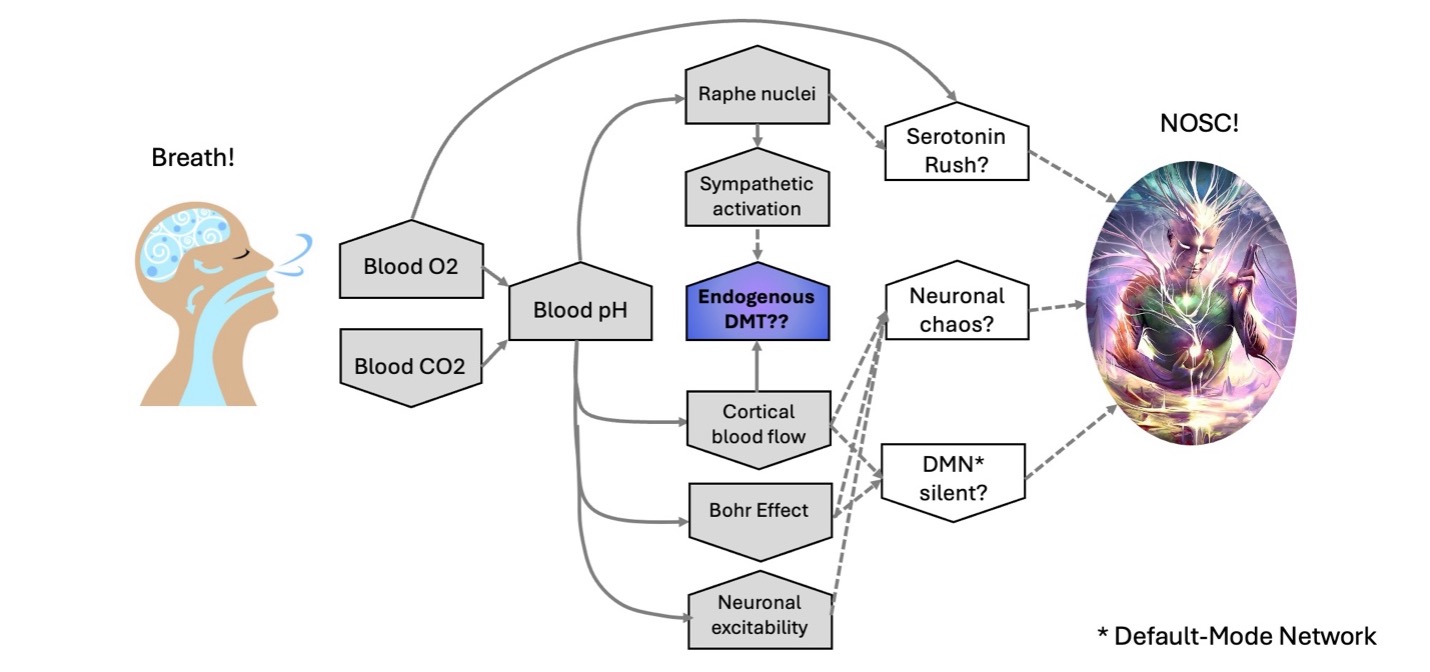
One of the first things that changes during breathwork is that the O2 saturation of your blood shoots up by about 40%, while CO2 saturation drops by about 50% [4][6]. Why? By breathing not only faster but also more deeply, you are boosting the exchange of O2 and CO2 in your lungs. As a result, your O2 supply is constantly refilled, while CO2 is removed more quickly. This in turn changes your blood pH – from its baseline value of about 7.4 (just above the neutral pH of 7.0) to a more alkaline, less acidic pH of 7.6 – 7.8 [7][8] . In case you have noticed a lack of exceedingly long words in your life recently: This phenomenon is known as respiratory alkalosis. Given that the entire pH scale goes from 0 (with gastric acid at about 1) to 14 (with bleach at about 13), a shift from 7.4 to 7.7 may not seem like much, but it is in fact pretty unusual. Our body likes its blood pH to stay almost exactly as it is, so typical pH values are clustered tightly between 7.35 to 7.45. In this context, a jump to a pH of 7.6 or even 7.8 is definitely newsworthy to your body!
Sympathetic Signalling
Your autonomic nervous system (ANS) is the part of your nervous system that orchestrates the things you can do without having to think about them, like sweating, pupil dilation, your heart beat – and indeed breathing when you are not controlling it consciously! These tasks are divided between two complementary ANS branches – the sympathetic (flight-or-flight) system and the parasympathetic (rest-and-digest) system. And as you may have guessed, circular breathwork is not mainly inviting you to rest and digest. When the CO2 levels in your blood start to seriously drop, several sympathetic actions kick in.
For one, adrenaline and noradrenaline production increases – by a whopping 360% and 150%, respectively, according to one study [9]! This in turn prepares your body for action in all sorts of ways: Your heart rate increases and your blood vessels constrict, leading to increased blood pressure [10][11]. And that’s not all – your pupils also dilate, your immune system wakes up, producing an extra 42% of lymphocytes, and your blood adds an extra 8% of thrombocytes, i.e. blood cells that seal off wounds, as well as about 10% more red blood cells [12]. In other words, your body gets ready to see what’s coming at you, to act on it decisively, and to quickly heal from wounds if necessary. Except of course that ‘what’s coming at you’ is in fact simply some intense breathing, but your body clearly takes that quite seriously.
Breathwork and the brain
Together, these physiological changes seem to be a crucial trigger for the NOSCs that breathwork can evoke. In a recent study of ours [4], we asked experienced breathwork practitioners to rate the depth of their experience throughout a session while we also measured their CO2 saturation. Falling CO2 levels were tightly linked with changes in consciousness: Without a drop in CO2, participants almost never experienced a full NOSC – and at very low CO2 saturations, nobody managed to stick to everyday consciousness entirely. Interestingly, low CO2 seemed to be a crucial first trigger for NOSCs, but once an NOSC had begun, it could keep going for a good while even once CO2 levels had returned to normal. In other words, physiological changes during breathwork are a trigger condition, allowing practitioners to enter NOSCs that then ‘self-maintain’ for a time.
How might physiological changes during breathwork push our brain to shift gears in this way? To answer that question, let’s first explore what our brain actually does during breathwork. Or at least, what it might be doing, because the science in this area is still fuzzy. One of the main reasons for this is a very practical one: While breathwork may inspire people to do many different things, ‘lying perfectly still with a fully relaxed face’ is typically not one of them. This poses a real obstacle, because basically any type of neuronal recording in humans requires participants to stay very still. Even small muscle movements, e.g. a smile or frown, can overpower the neuronal signals we are trying to record.
This makes the neuroscience of breathwork a tough nut to crack. The first study we found that dared to directly analyse neuronal activity during circular breathwork was conducted by Sviderskaya & Bykov (2006) [13]. In this study, EEG signals were recorded throughout a one-hour long breathwork session, and afterwards, participants were asked to give detailed accounts of their subjective experiences. These recordings showed that during breathwork, the synchronization between brain areas generally declines, meaning that neuronal activity from different areas does not occur together or stick to the same rhythm. At the same time, slow oscillations (i.e. activity waves running slowly through the brain like a Mexican wave in a football stadium) became bigger all over the place.
After this first breakthrough study, neuroscience took a break from the topic – the next papers exploring the neuronal signatures of breathwork only popped up almost 20 years later! Bahi et al. (2024) [5] collected EEG recordings before and after breathwork (not during! So no pesky issues with recording quality!). In an intriguing contrast to Sviderskaya & Bykov (2006), they found that slow neuronal oscillations actually got smaller after breathwork, while fast oscillations became bigger.
Then, just a few months later, Lewis-Healey et al. (2024) [14] gave their study participants small, portable EEG recording systems to use at home while taking part in SOMA breathwork sessions with online guidance. Now, online-guided SOMA breathwork may be slightly more meditative than some other flavours of circular breathwork, but it is definitely part of the circular breathwork family! So Lewis-Healey et al. is to our knowledge the second study to record neuronal activity during circular breathwork. Based on the ‘home recordings’ they collected, Lewis-Healey et al. reported reduced slow neuronal oscillations during breathwork – similar to Bahi et al. (2024) and unlike Sviderskaya & Bykov (2006). What’s more, they found some fascinating parallels between the neuronal fingerprints of breathwork and of psychedelics, especially a clear decrease in the predictability of neuronal activity – or in other words, an increase in chaos. More on that later!
These studies give us a first, intriguing glimpse at the brain dynamics that go along with breathwork experiences. And yet, much of the story remains untold so far. For instance, increased slow oscillations are also seen during sleep [15][16]. So the neuronal changes reported so far have not yet revealed the crucial aspects of neuronal activity that support the unique experiences sparked by breathwork.
Psychedelic research to the rescue
So here we are – with a decent idea of what breathwork does to our body, a bit of insight into what it does to the brain, and no clue how to get from one to the other. If we want to know more, we will have to pull ourselves out of the swamp of having-no-clue by our own bootstraps. And the best bootstraps we can find in this case are other NOSCs, especially those induced by psychedelics. As we have discussed at the start of this post, breathwork experiences show some real similarities with psychedelic states; their long-term effects also decidedly overlap, and even the little we know about the neuronal fingerprints of breathwork seems to resemble psychedelic states (see above). Based on these clues, we might assume that the brain states of psychedelic and breathwork experiences are at least somewhat related. Now, this is mostly guesswork, and similar subjective experiences can also be reached by taking quite different routes through the brain. But since this is the bootstrap we have chosen to hang our scientific quest on, let’s pretend that this is definitely true! If brain states evoked by breathwork and psychedelics are similar, what should that look like? Well, not all psychedelic states are created equal, but there seem to be three fundamental qualities that have been documented consistently across different psychedelic states: Serotonin release, quieting of the default-mode network, and neuronal chaos!
Serotonin as key trigger
Even though different psychedelic substances target somewhat different sets of neurotransmitters [17][18], Serotonin seems to play a central role in pretty much all of them. In other words, it is hard to trigger a psychedelic experience without hitting at least a few Serotonin receptors of one kind or another. Could breathwork do this as well? Based on what we know, that is definitely possible.
The Raphe nuclei
During breathwork, your rising blood pH will be picked up by sensor cells registering gas concentrations in the blood that’s passing through your carotid artery (the one in your neck that comes up a lot in stabby movies). This info is passed on to a whole host of neuron groups in the brainstem that help to adapt your breathing to your needs. Many of these nuclei are especially triggered by high CO2 and low blood pH, because this typically means that you are in danger of suffocating. Nevertheless, some areas, like the Raphe nucleus obscurus, also respond to the unusually low CO2 and high blood pH that you encounter during breathwork. When CO2 saturation falls, neurons in the Raphe nuclei start ramping up their activity until you slow down your breathing [8]. Which is probably also the reason why many people experience an urge to stop breathing somewhere around the 10-minute mark of a breathwork session. Your Raphe nuclei are telling you to cut out this weird circular breathing stuff!
Now, if you keep breathing intensely despite the stop signals from your raphe nuclei, it stands to reason that they may start ramping up their response. If this is true, it would probably have two knock-on effects: First, the Raphe nuclei are in the perfect position to activate the sympathetic nervous system (see above). Second, all seven Raphe nuclei are at least somewhat interlinked, so when circular breathing triggers activity in the ‘lower’ Raphe nuclei, this activity may spill over to the ‘upper’ Raphe nuclei – and those are the central source of serotonin for the entire brain. Such a mechanism has neither been tested nor proven, but it’s one potential way in which intense breathing might push your Raphe nuclei, and thereby your entire brain, into high serotonin release.
Oxygen makes Serotonin
Another way in which breathwork might boost serotonin release comes from research by Nishikawa et al. (2005) [19], who showed that higher O2 levels in your blood lead to higher serotonin release across the brain. The reason is that when more O2 is available, your brain can use that to produce serotonin. In their experiment, Nishikawa et al. saw a dramatic 50% increase in serotonin when people breathed air with a 15% versus 60% O2 content. Which may also explain why breathing more deeply in every-day life makes you happier! Now, below we will discuss a couple of reasons why more O2 in the blood may not necessarily translate to more O2 for the brain – so this mechanism may or may not work well during breathwork. However, the fact that the Raphe nuclei sit in the brain stem – which is one of the areas with the steadiest blood flow – makes this at least a possibility.
For an exciting bonus avenue for extra Serotonin signalling during breathwork, read on to the end of this post!
Shutting off the default-mode network
Another common feature of psychedelic states is that the transition out of your every-day consciousness comes with a hush in the cortical areas involved in planning, predicting, evaluating, and all the other ‘commentary on life’ we tend to keep running in our head [20]. Many of these areas are part of the default-mode network (DMN) – a web of interconnected brain areas that together construct much of what we experience as ‘me’: Defining our self-image, remembering our personal history, predicting and planning our personal future, and computing how others see us [21]. During psychedelic states, some of the DMN’s central hubs, like the posterior cingulate cortex and the medial prefrontal cortex, quiet down [22][23]. On top of that, communication within the DMN, as well as between the DMN and the rest of the brain, is severely messed up [22][24]. And this is not just a temporary effect – communication within the DMN can stay choppy for weeks after a psychedelic experience [22][25]; and regular users of psychedelic substances like Ayahuasca show a permanent thinning of neuronal tissue in the posterior cingulate cortex [26]. Put more poetically, psychedelic states make it harder for your brain to keep telling you the rehearsed story of who you are. How might similar changes happen during breathwork? Here are some ideas.
Food for thought
As your blood CO2 drops, your brain starts closing its doors to all this weirdness [27]. More specifically, it closes its arteries. Even more specifically, it constricts them, cutting blood flow by up to 50% – the less CO2 in your blood, the less blood gets through to your brain [7][11]. What’s more, this happens in a highly selective way: While blood flow decreases somewhat in the whole brain, the most affected areas generally sit in the neocortex (i.e. your ‘thinking’ brain), with a few areas from your mesocortex (i.e. your ‘feeling’ brain) thrown in [28][29]. When you look at those areas more closely, a lot of them (including the ever-intriguing posterior cingulate cortex) are in fact part of the DMN. Which means that by reducing the CO2 saturation of our blood, we may be putting a bit of a natural strangle-hold on our DMN.
This strangle-hold may become even more strangly because of the so-called Bohr Effect. The Bohr effect is a really cool way of distributing O2 across the body according the old Marxist principle ‘From each according to his ability, to each according to his needs’. It works like this: Your blood doesn’t just randomly deliver O2 everywhere. Instead the haemoglobin in your blood decides where to set free the O2 molecules it is carrying. And it does that according to our old friend, the blood pH. At each moment, different parts of your body, including your brain, may be active to different degrees. And the more active they are, the more CO2 they produce, and the more sour the blood pH in the neighbourhood. Because of this, under normal circumstances blood pH is a good proxy for how active a body part is at the moment, and how much O2 it therefore needs. And your blood responds to that demand: haemoglobin holds on to O2 molecules when it’s in an alkaline environment, but sets them free in acidic environments. That way, O2 reaches the busiest body parts first. That’s normally a remarkably elegant system to distribute energy – until someone starts to breathe intensely for a while and thereby alkalinising their blood. This puts your body, and especially your thinking brain, in the somewhat ironic position that your blood is brimming with O2 , but little of that O2 ends up making its way to your thinking brain. While this is not medically dangerous for healthy people, it likely limits the neuronal activity your thinking brain can generate during breathwork – and that may help to remove some of the mental filters we usually put on our experience of the world.
Anarchy!
Do you love anarchy? Your brain on psychedelics certainly does. During psychedelic states, neuronal communication becomes more flexible and chaotic, both in time and space. In time, because the dynamics of neuronal activity, i.e. the timing at which different neurons and brain areas get fired up or fall silent, becomes less predictable [30][31]. In space, because the way activity flows from one brain area to another becomes more promiscuous and flexible [23][32]. Communication between brain areas also becomes less hierarchical, so that ‘higher’ executive areas like the ones in the DMN shut up more, while ‘lower’ subcortical and cortical areas processing sensory information get more of a say [33]. This even includes the simultaneous activation of the sympathetic and parasympathetic nervous system, which would normally be more prone to taking turns than working in parallel [34]. In other words, everyone talks to everyone at the same time!

The findings by Healey et al. (2024) give a first hint that breathwork might be able to trigger similarly ‘anarchic’ brain states: As mentioned above, they showed that rhythmic activity from different brain areas was less synchronized and more diverse (i.e. unpredictable) during breathwork. How might such chaotic neuronal activity come about during breathwork? Well, the mechanisms we discussed above seem to be collaborating on a sort of neuronal Robin Hood scheme, taking from the rich and giving to the poor: They increase general neuronal excitability, but at the same time shut off O2 supply to higher executive brain areas. As a result, all brain areas should have a more equal chance to communicate – also along the pathways that may not be quite as well-trodden. On top of that, if Serotonin release increases during breathwork, this could add an extra layer of general cross-area excitation beyond the usual communication pathways [18][35]. Finally, another interesting effect of alkaline blood is that neurons get very, very excited by it. That likely adds a sort of ‘blanket of extra activity’ on top of the usual neuronal responses. This added excitement also accounts for the muscle cramps (tetany) we mentioned before – when the neurons driving your muscles become more excited, they will make your muscles cramp up [36]. This increased neuronal excitability seems to outweigh at least some of the silencing effects that should come with reduced blood flow (see above), especially in subcortical areas. It can even trigger seizures in patients who have a history of epilepsy [37] – which is the reason why epilepsy is one of the strongest contraindications for breathwork.
The Joker: Endogenous DMT
Together, these processes may already be powerful enough to trigger neuronal dynamics similar to those observed in psychedelic states. Alternatively, they may also be getting some extra help from endogenous dimethyltryptamine (DMT), i.e. DMT that is produced by the brain itself. DMT is one of the oldest psychedelic compounds known to humanity, ingested by smoking or as part of psychedelic brew like Ayahuasca, which has served spiritual and therapeutic purposes in Amazonian communities for centuries and possibly millennia. In the brain, DMT activates Serotonin receptors – in fact, it is better at lighting up Serotonin receptors than Serotonin itself [38]! And as one of the classical Serotonin-based psychedelics, it also triggers all the neuronal dynamics that are most typical of psychedelic states [39]. As such, if breathwork could cause the brain to produce DMT, this would very much explain why breathwork experiences and psychedelic states seem so similar!
That would be an elegant story, but we don’t know yet if it is true. The question whether the brain brews its own supply of DMT for special occasions has been hotly debated for decades, and a clear answer is not yet in sight [40]-[43]. Your body definitely has all the ingredients that are needed to cook up DMT [43]-[45]. The question is just whether it actually brings those ingredients together in your brain. And if yes, the next question is whether such brain-grown DMT is produced in small bits here and there for ‘housekeeping’ e.g. to protect and repair neurons [40][46][47] – or if it can also show up in quantities that can seriously shift your consciousness [43].
That is especially difficult to find out because even when DMT is produced in the brain, the typical time it spends in the brain before being pulled apart again is six minutes [40]. And even if one could measure DMT fast enough before it falls apart, it will probably not be produced equally all over the brain – which means one would need to know where exactly to go looking. Together, these obstacles make brain-grown DMT hard to catch in the act.
Which brings us to the most interesting question: How likely is DMT to show up in your brain during breathwork? There is one really cool reason to believe that this may be the case. It just so happens that the molecule that keeps disassembling DMT, which is called MAO, really likes O2. Without O2, MAO stops slicing DMT into bits; which means that DMT sticks around in higher amounts [40][47]. And this in turn allows DMT to sneakily sabotage MAO production, starting a feedback loop of growing DMT concentration [48].
Why would the brain have a mechanism to increase DMT concentrations during O2 shortages? Because apart from moonlighting as a psychedelic, DMT appears to work a few other jobs in the brain. This includes protecting neurons from O2 starvation [49]. So, whenever your brain is missing O2, it might start producing DMT as a neuronal shield. Now, remember what we said above about blood flow, and O2 availability getting restricted during breathwork? And how this restriction is especially targeted at crucial hubs of mental control like the prefrontal cortex?
If we put these bits of information together, the following picture emerges: During breathwork, internally produced DMT starts to accumulate especially in brain areas with low cortical blood flow, because in those areas, it cannot be fought by its arch-enemy MAO. This includes prefrontal, parietal and cingulate cortex, which also happen to be the areas that get most dramatically impacted by other NOSCs. Coincidence? I think not, dear Watson. And with this flourish of wild speculation, let’s summarize!
Wrapping it all up
It seems that breathwork puts your body into a quite an unusual physical state that we might call a ‘happy fight-or-flight mode’ – your sympathetic nervous system is pumping, blood flow to your cortex is down, but at the same time you are likely releasing more Serotonin. This slightly whacky constellation puts you in a good position to hit a lot of the classical neuronal fingerprints of (psychedelic and other) NOSCs: (1) Serotonin flooding, which might happen both because of the Raphe nuclei, because of high O2 saturation, or because endogenous DMT hits Serotonin receptors like a freight train. (2) Quieting of the DMN, which might be achieved by decreased blood flow, boosted by the Bohr Effect; and (3) Unpredictable cross-talk between neurons across the brain, which might be supported by the increased excitability of neurons, and by the fact that your ‘feeling’ and ‘survival’ brain are less affected by restricted blood flow, giving them the chance to mount a revolution against the ‘thinking’ brain areas at the upper end of the cortical hierarchy.
Now, while these are very exciting stories, at this point, they are really just that – stories. Hopefully not bad or crazy ones, but untested for sure. In the coming years, we are excited to see (and contribute to) work that starts to explore these fascinating dynamics through the lens of science. In the meantime, you definitely don’t need to understand all the neuronal workings of breathwork in order to try it. So if this has made you curious, we invite you to breaaaaathe deep, and experience for yourself how changing your breath can change your mind!
Happy breathing!
Martha & Abdel
P.S. If you want to experience breathwork and altered states of consciousness in a safe setting, you might find this article useful: “How to recognize a quality retreat in 2025” or dive into our “Deep inner work series“, to explore the traditions of thought and practice that shape the Evolute approach.

Patrick Liebl,
Lead Facilitator & Integration Expert
Curious to learn more?
We invite you to schedule a call with us. Together, we can explore any questions you may have. We can explore whether a program with a legal psychedelic experience is right for you at this time.
“We are here to support your exploration, at your pace, with no expectations.” – Patrick Liebl